Healthcare IT | 10 May 2023 | 12 min
The Power of Telemedicine: How Going Remote Can Revolutionize Healthcare

Telemedicine has become a new normal since COVID confined us to our homes. It is an evolving strategy that is changing the way the world operates today. It is patient centric and concentrates on health rather than illness. It is a tool for patients to:
Let’s consider these reports:
After reading these reports, I decided to write a blog about the applications and opportunities of telemedicine. These are for both patients and providers.
Also, this blog will highlight the challenges associated with implementing telemedicine. It will also focus on some of my recommendations to overcome these hurdles.
Let us start with the most obvious question – Why Telemedicine?
Industry experts and studies continue to point toward telemedicine as a means to:
Telemedicine is required to:
Telemedicine is not a new concept. In fact, it has its origins traced back to the early 20th century where healthcare was provided by remote Information and Communication Technology (ICT).
But technological (transferring video, audio, or images) and financial shortfalls then did not allow it to go into full bloom.
Though a century has gone by, Telemedicine is still in its nascent stage, and it seems to encounter quite a few challenges on the way:
I will talk about how you as a Healthcare provider can enhance patient care by tiding over all these challenges in my last section.
But let’s talk now about Stanley Kubrick vs Steven Spielberg! (Tch… of course the former. Just kidding, let’s talk about why Telemedicine and Telehealth may seem, but are not the same thing.)
In the healthcare industry, the terms “telehealth” and “telemedicine” are often used interchangeably. Even the ATA (American Telemedicine Association) considers them to be interchangeable terms.
I won’t be too surprised by this because both Telemedicine and Telehealth have eerily similar definitions. A lot of services overlap, viz.
Telemedicine is a subset of Telehealth. Telehealth includes all health services provided through telecommunications technology. Meanwhile, telemedicine sticks specifically to clinical services.

Fig 1: Telemedicine v/s Telehealth
To put it more simply, Telemedicine is like having a direct line to your physician or care provider. This way, you can text, video call or chat with them about your condition. They, in turn, can care more for you, monitor you, and send you your reports.
On a side note, the CMS (Centers for Medicare & Medicaid Services) has identified CPT (Current Procedural Terminology) codes. This is for Telehealth and Telemedicine to ease the reimbursement process for providers. There are incentives for Telehealth and Telemedicine under the CPC+ (Comprehensive Primary Care) program.
Telemedicine can offer a variety of enhancements in telecommunicating with a physician or a care provider. Here are some requirements for telemedicine to be successful.

Fig 2: Core requirement and value add requirements for telemedicine to be successful
Some more requirements to give you the whole picture:

Fig 3: Some more requirements for telemedicine to be successful
In my next section, I thought it would be a good idea if I grazed the current scene in telemedicine, instead of delving deep. This is because a chart can say a thousand words.
Video-based consultations have been on the rise. These are perhaps more used now than they were a few years back:
Smartphones jumped onto the Telemedicine bandwagon sooner than we ever anticipated.
Research shows that about 30% of people already use mobiles to check their diagnostic information. So, mHealth apps provide real-time inspection. Patients can even chat about their symptoms with their physicians.
I did briefly state this example when talking about Telehealth. But wearable devices are where the lines blur between Telehealth and Telemedicine. These have taken monitoring of patients to the next level. They monitor and capture vital parameters continuously. They also relay statistics to the patient’s smartphone via Bluetooth.
I remember when a friend told me about how he received timely treatment because his device alerted him of a probable heart attack. Even now thinking of it makes my stomach churn in such a way that it may probably be apologizing to the other organs in there. That is perhaps the power of technology. (I meant the wearable device alert if you were lost because of what followed.)
Getting back, the table below shows what kinds of technology can be used during remote treatments. A COVID 19 barometer study by Sermo, found that 63% Healthcare practices in the US used these technologies during the COVID 19 outbreak.
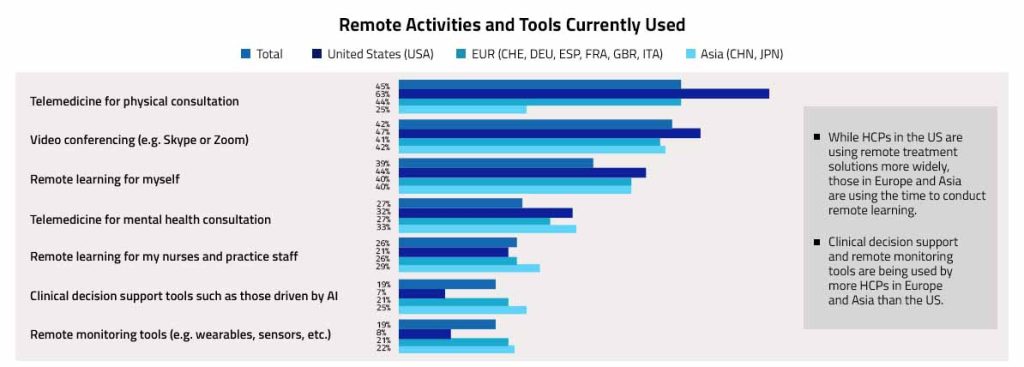
Fig 4: Technologies used by healthcare practices in the US during the COVID 19 outbreak
Any telemedicine solution should be able to break through the challenges I mentioned earlier in this blog. It should possess a video and audio-conferencing capability having the right encryption and security in place as per HIPAA guidelines.
It should be capable of sending and receiving images while complying with healthcare standards. Such a solution should easily integrate with your existing EHR or PMS system. This is so that a provider can refer to patient’s medical record.
Technically speaking, a solution should have an AES264 encryption for security with STUN, TURN communication, and FIPS server. What’s more, it should be able to integrate with any system via API.
With advancement in technology and us inching towards Industry 5.0, Telemedicine has the capability to be a robust technology. It is taking Healthcare IT to a new level. So, Telemedicine, I think, may well be on its way to be the evolution of healthcare.
You can write to us if you would like to know about how adopting a more specific approach to Telemedicine will help your healthcare company to enhance patient care. Also visit us at Nitor Infotech to know about the services we have to offer.
we'll keep you in the loop with everything that's trending in the tech world.
