Digital Transformation | 03 Jul 2020 | 14 min
Why is there a need to drive Digital Transformation into Palliative Care?

Health is a state of complete physical, mental, and social well-being and not merely the absence of disease or infirmity. The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being.
There has always been a lingering question around Palliative care-has there been enough integration of digital technology in all areas imaginable, is there something more that can be done to improve end of life experiences?
Palliative care is developing faster than we can imagine and decision makers face two of the most important challenges –
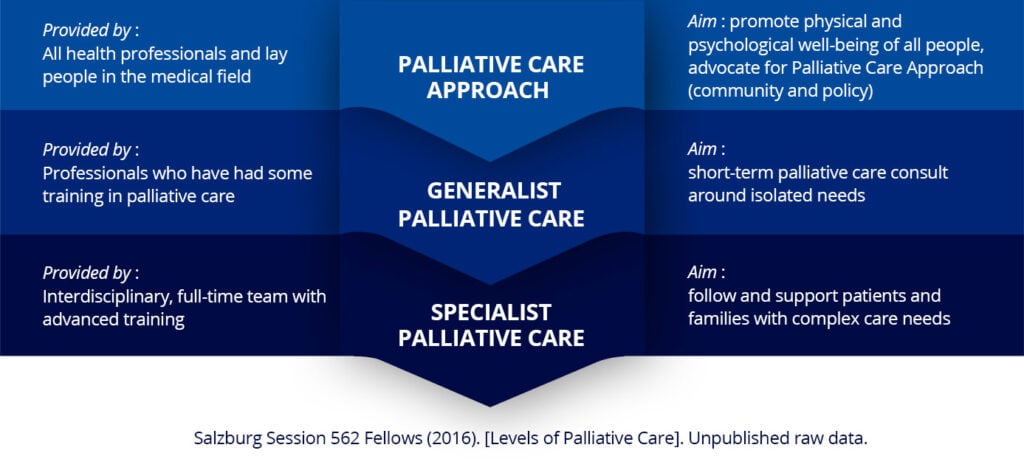
Data integration effectively integrates hospices, palliative care services, and local healthcare services to support and comfort patients with palliative care needs and improves care delivery across the care continuum.
Technology integration is that missing piece in the jigsaw puzzle of effective use of home health care. Be it appointment tracking of patients or devising long-term care strategies, this is perhaps the key to both patient satisfaction and high quality care. The more the information available with just a few clicks the easier the lending of care becomes.
So in order that patients are cared for better, and providers can care better, we need data integration. Over the course of this blog, I will also talk about who needs to have data integration in place, and what kind of solution can actually help make this a reality.
It is not easy for families to look at all the medical needs of a patient and also say their final goodbyes with equal ease.
So how can healthcare providers use innovative technology to help patients receive better care, and families spend more time with their loved ones, and in all this-how can data integration actually be the answer they are looking for?
Here is why data integration can actually help:

To reiterate the need for effective use of data, I would like to draw a parallel to a study conducted by the New England Journal of Medicine.
The study focused on patients newly diagnosed with metastatic non-small-cell lung cancer. The results showed that patients who received standard oncological care and met clinicians frequently had a better quality of life, lower rate of depression, and had a survival benefit of 2.7 months.
This means that through early diagnosis, timely intervention, strong and personalized patient support, increased scope of care, and streamlined operations, technology integration for home health care becomes an achievable and potentially beneficial goal.
A report states that global Big Data in the healthcare market was $11.45 billion in 2016 and will have double digit growth by 2025.
The report also added that healthcare data volume surged to over 700 exabytes in 2017 from 153 exabytes in 2013, and is estimated to grow to 2,314 exabytes by late 2020. According to the report, the factors that can contribute to the growth, to name a few, include emergence of cloud-based services and subscription models, government initiatives encouraging adoption of healthcare information systems, mHealth, eHealth, and wearable technologies.
Here is a diagram that best illustrates the sectors that need data integration for improved quality of care.
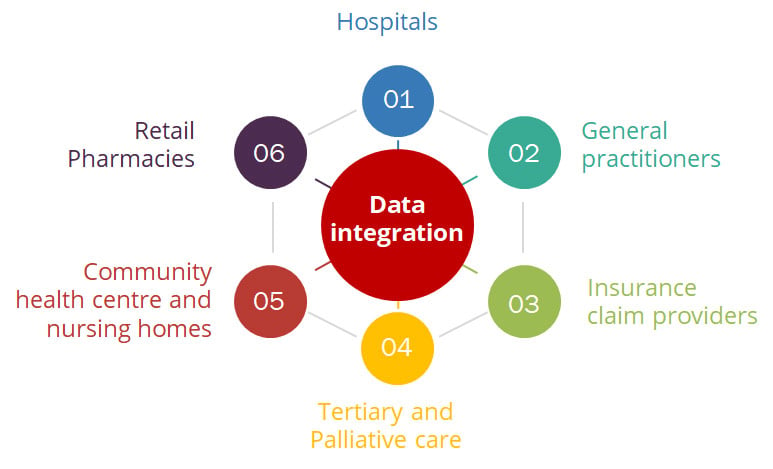
Hospitals and healthcare organizations will have to prioritize their investments and focus on improving patient outcomes. Ever mounting healthcare costs, increasing number of chronic diseases, aging population, and reducing reimbursement costs will necessitate this very investment. The supply of health-related data from various data points can transform healthcare, provide value-based care, improve patient outcomes, and reduce costs.
By having patient information from different care locations in real time and in a single place, data integration-a wider term being interoperability-has given a true picture of what a patient actually experiences.
Providers need to turn to data integration when they:
Data integration requires truly integrated systems, ones that can exchange data and present it in a comprehensive manner on a user-friendly interface.
This is a standard data integration approach:

In conclusion, the aim of data integration for palliative care should always be to improve care for patients and their families, alleviate the burden of symptoms, and improve the quality of life.
Improving digital systems like the EHR can go a long way in improving the ability of the clinical staff to work efficiently. By identifying palliative care patients or home health patients needing hospice care early through predictive analysis, we can ensure that patients, their families, and providers have conversations much sooner so that the right care is delivered at the right time.
It is important to use data meaningfully so that it can in turn influence healthcare policy and clinical care. With the right technology, closing gaps, reducing errors, and improving quality of life becomes possible. For the future of palliative care, greater access to health information and better ways of data exchange are needed. With little time in patients’ hands, we will need to help them make the most of it through technology.
Nitor Infotech has successfully used data integration techniques by helping clients make meaningful use of data, write to us to know more about our services.
we'll keep you in the loop with everything that's trending in the tech world.
